What is a diabetic foot ulcer?
A diabetic foot ulcer is an open wound that takes a longer time to heal due to vascular disease or elevations in blood glucose levels. Foot ulcers in patients with diabetes should be treated immediately to reduce the chance of infection that may lead to amputation, which ultimately could result in the deterioration of function and quality of life.
What are the causes?
Ulcers can be caused by the length of time you have had diabetes, poor circulation, foot deformities and trauma/irritation to the skin caused by friction or pressure.
People who have had diabetes for long durations often develop neuropathy due to nerve damage, causing them to have reduced or a complete lack of feeling to the foot,
making it harder to spot any foot health issues as there will be little or no warning pain. It is therefore extremely important to make sure you thoroughly check your feet for any signs of broken skin or sores.
What are the symptoms?
Symptoms include drainage, bleeding, redness or swelling and if the wound has progressed significantly there may be a noticeable odour.
When do I seek medical attention?
As soon as you notice an ulcer forming, contact your GP immediately. No matter how small or insignificant you think it may be, it is always better to have any abnormalities checked and treated as quickly as possible to increase healing time before any infections may arise.
What is the treatment process?
The primary goal is to heal the wound as fast as you can before an infection has time to form. If your GP diagnoses an infection, a treatment program of
antibiotics, wound care, and a possible trip to your local diabetic wound care clinic may be necessary. However, not all ulcers will become infected.
What to expect - Treatment:
- You may be prescribed a wheelchair / crutches or other forms of foot brace or specialised castings to take the pressure off the affected area. This will promote faster healing.
- To prevent infection, your GP may prescribe specialist medication or apply dressings to the ulcer.
- Your GP may create a management plan to control blood glucose levels and other health problems.
- It may be required to remove dead skin and tissue, known as "debridement".
- Surgical options: Most non-infected ulcers can be treated without surgery, however, if this treatment is unsuccessful, surgical management may be needed. This may include shaving or excision of bone(s) and the correction of various deformities, such as hammertoes, bunions, or bony "bumps" may be necessary.
After treatment - Avoiding infection
- Wounds and ulcers heal faster with a lower risk of infection if they are kept covered and moist.
- Keep the ulcer clean and bandaged.
- Clean the wound daily, using a wound dressing or bandage prescribed by your GP.
- Avoid walking barefoot.
- Keep blood glucose levels under tight control.
- If prescribed, orthotic footwear should be worn as directed to help reduce the risk of future ulcers.
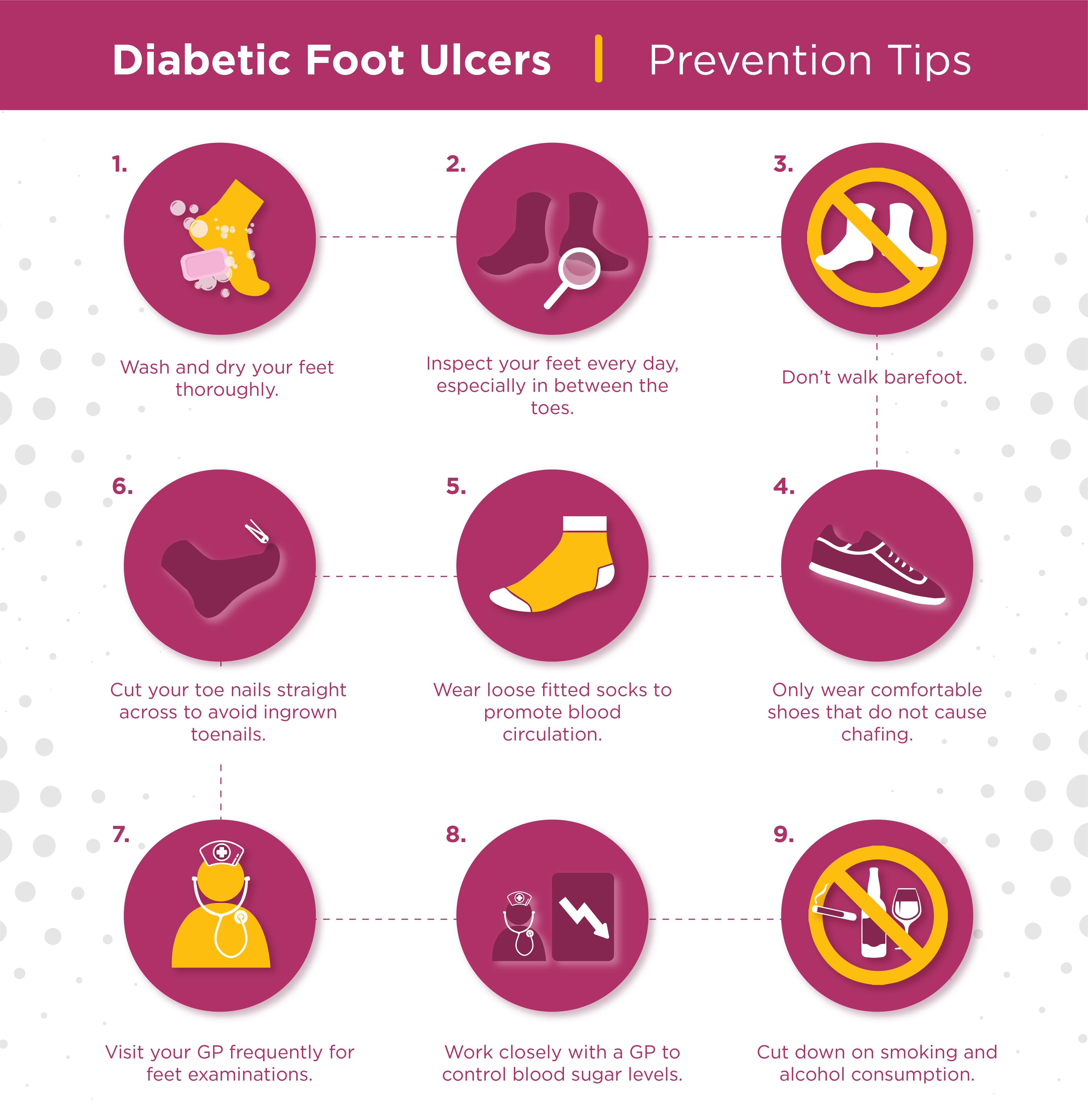
In conclusion, it is extremely important to check your feet regularly and consult your GP at the first sign of any abnormalities. If you are concerned about your feet you can find your local Podiatrists and Chiropodists services here. Below we have included a handy prevention tips infographic for you to download for future reference.